This week, Health Minister Mark Butler cut through the lobbying and made a decision that (could) justify the entire spending on the My Health Record System. Dr James Freeman explains how and why.
Hallelujah, praise the Lord and pass the ammunition. This week, our Health Minister, Mark Butler, cut through the lobbying and made a decision that could justify the entire spending on the My Health Record System. How so? First, let’s look at the what…
The long form of what is here in a speech from the Minister. Now let’s look at the why? Underlying Minister Buttler’s decision is this trend:
Over the past four decades, our government has consistently funded over 90% of all pathology spending. Over the same period, GPs like me and other doctors have ordered not 1x, not 2x, not 3x, but rather 5x more pathology services, excluding the COVID blip when we got to 7x.
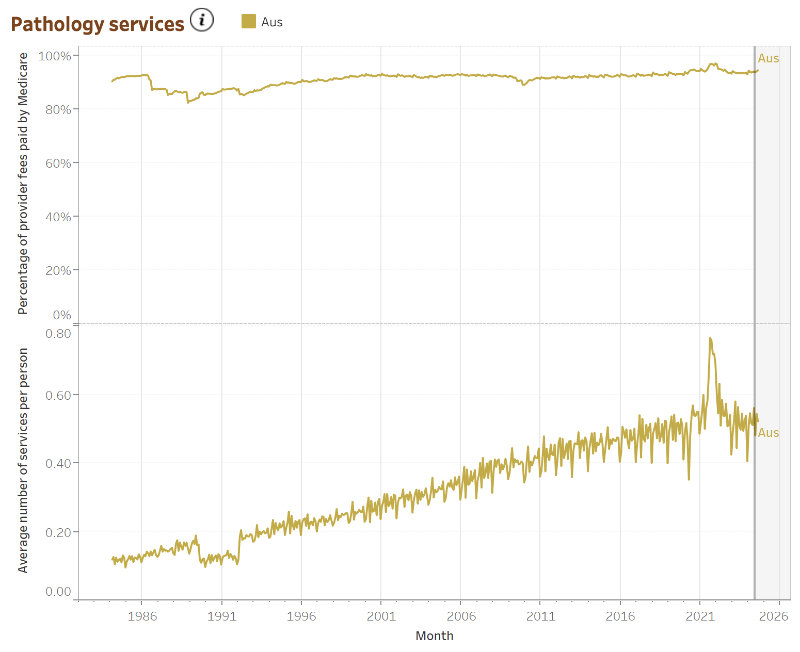
Source: AIHW.gov.au
Why? Our ageing population is one reason. Why? Because we doctors are all terrified of missing something rare. Why? Because we, the people, and the no-win, no, no-fee lawyers insist that we do.
And we, the people, spent $3.72B on pathology in 2023/24. Although given a total health budget of $140+ billion, this must surely be down to the paperclip end of the spectrum?
Perhaps, but given that all GP services run to a little under $10B, all medications are a little over $10B, and all radiology is about $5B, pathology remains a big ticket item in the primary care arena.
So, let’s take a very quick look at the backstory before we get to how the pathology companies hoodwinked the government.
NEHTA
The National E-Health Transition Agency (NEHTA) was established by the Australian government in 2005 as part of an effort to create a cohesive national approach to health information technology and to streamline the healthcare system through electronic health services.
The key milestones were:
- Formation and Early Development (2005-2011):
- NEHTA focused on building foundational digital health structures, such as standardized health information exchange protocols and unique healthcare identifiers (for patients, providers, and organizations).
- Introduction of My Health Record (2012):
- In 2012, NEHTA helped launch the Personally Controlled Electronic Health Record (PCEHR), later renamed My Health Record (MyHR).
- This national digital health record system aimed to improve care coordination and reduce unnecessary duplication in the healthcare system.
- The initial uptake was slow due, in part, to privacy concerns, and adoption remained low.
- It was, in short, a gigantic white elephant.
- Expansion and Transition to the Australian Digital Health Agency (2016-):
- In 2016, NEHTA it was replaced by the Australian Digital Health Agency (ADHA) who assumed responsibility for expanding the My Health Record initiative, making it opt-out in 2018.
- This increased the number of active digital health records from 10% to 90% of the population.
Back in the 2010s, I was busy establishing GP2U Telehealth, and part of that process included taking a million-dollar investment from Sonic Pathology. This made me privy to some of their internal banter, such as, “When NEHTA asked us for atomic records, we said no, but we can do PDFs. We expected pushback, but it never came.”
It’s fair to say I was probably not the only person who reflected that NEHTA could not fight its way out of a wet paper bag.
So, what are “atomic records”? Why are they good, and why are PDFs bad?
Health Language
For the past 3 decades, pathology results have been presented to practice management software as atomic records in a format called Health Language 7 (HL7). Here is an example of HL7 dating back to 1987.
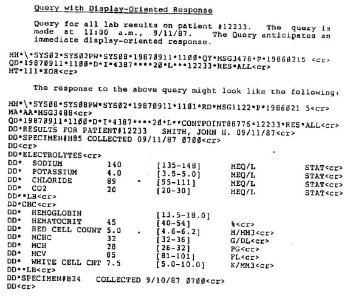
HL7 record
Fundamentally, one database spits out some HL7, which another database can then absorb. As you can see above, there is patient identification information, and then each result is a line item.
This is atomic data, and HL7 is designed to facilitate data transfer from one database to another. It predated NEHTA by two decades and was in routine daily use by every pathology company in Australia in 201x.
So, how do things work right now? Pathology providers dump data into buckets that are accessible by the requesting doctor.
Every 15 minutes, the practice management systems in Australia query the relevant pathology providers for data that relates to them and drain the data buckets.
That data then appears in the PMS for the doctor to mark off as received and take appropriate action. As new results are generated, the buckets are refilled, drained, etc.
Implementing this for MyHR use requires very little work. Pathology providers use their existing systems to dump ALL their result data in a bucket marked MyHR. Every 15 minutes or so, or during off-peak hours, the MyHR drains the bucket and puts it into the record.
There is work required, and that work is mostly at the MyHR end, where some knowledgeable people who understand the purpose of this data and how doctors need to see/use it should be engaged to help.
Very little work is required at the pathology end. I would hazard an educated guess it costs the pathology companies far more to implement the current broken PDF system rather than expand on the existing HL7 atomic record, data bucket, and data download system.
Why does it matter?
For pathology companies, the issue is simple. As things stand, it is cheaper for me (as a doctor) to reorder a test than to make 3+ phone calls trying to retrieve data from one of the 3+ local pathology service providers.
The underlying statistic is that 20% of all pathology tests done were already done in the prior 60 days by a different doctor. While many of these tests may well have been indicated due to a change in the patient’s condition, there is little doubt that it is faster for a GP/Specialist to order a test again than to see if there is a recent result available.
~20% of $3.72B is a ~$750m a year saving,
achieved by avoiding pointless duplication of pathology testing.
The big picture questions about privacy vs utility and do we trust the government with our data remain ever relevant. Still, they should be considered against the reality that Sonic Healthcare, Healius, and Australian Clinical Labs (ACL) already hold all this data and having it sent to me is as simple as a phone call.
Would patient care be better if doctors like me had oversight of all a patient’s pathology? I suggest the answer is yes and applaud the Minister for his courage in addressing this issue.
Dr. James Freeman is the founding owner of GP2U Telehealth and an executive director with responsibilities for platform development and clinical oversight. He brings 20 years of clinical and information technology experience to the company.
James has a B.Sc. and MB,BS from UTAS and is on the Dean’s Roll of Excellence for outstanding academic achievement.

